journal articles
Publishing in academic journals is an important part of academic research because articles are reviewed by independent experts.
Academic journal articles are a good place to go into more in-depth analysis of our data than we could do in a community report or a fact sheet. These are also a good way for our findings to reach other academic researchers and health professionals.
Our aim is to make as many of these freely available to the public as possible.
- Push and pull factors of transgender migration to Aotearoa/New Zealand
- Eating disorder risk in transgender youth and its association with unmet need for gender-affirming hormone therapy in Aotearoa New Zealand: a cross-sectional study
- The glue that binds us: The positive relationships between whanaungatanga (belonging), the wellbeing, and identity pride for takatāpui who are trans and non-binary
- Perceived legal protection and institutional trust predict a lower psychological distress level for transgender people in Aotearoa/New Zealand
- “It’s just a general lack of awareness, that breeds a sense that there isn’t space to talk about our needs”: barriers and facilitators experienced by transgender people accessing healthcare in Aotearoa/New Zealand
- Transgender-related stigma and gender minority stress-related health disparities in Aotearoa New Zealand: hypercholesterolemia, hypertension, myocardial infarction, stroke, diabetes, and general health
- Uptake, experiences and barriers to cervical screening for trans and non-binary people in Aotearoa New Zealand
- Unmet need for gender-affirming care as a social determinant of mental health inequities for transgender youth in Aotearoa/New Zealand
- PrEP awareness and protective barrier negotiation among transgender people attracted to men in Aotearoa New Zealand
- Barriers to possessing gender-concordant identity documents are associated with transgender and nonbinary people’s mental health in Aotearoa/New Zealand
- “I teach them. I have no choice”: Experiences of primary care among transgender people in Aotearoa New Zealand.
- Supportive interactions with primary care doctors are associated with better mental health among transgender people: Results of a nationwide survey in Aotearoa/New Zealand
- Gender identity change efforts faced by trans and non-binary people in New Zealand: Associations with demographics, family rejection, internalized transphobia, and mental health
- Access to fertility preservation for trans and non-binary people in Aotearoa New Zealand
- “Being trans intersects with my cultural identity”: Social determinants of mental health among Asian transgender people
- “It’s how the world around you treats you for being trans”: Mental health and wellbeing of transgender people in Aotearoa New Zealand
- Enacted stigma experiences and protective factors are strongly associated with mental health outcomes of transgender people in Aotearoa/New Zealand
- Mental health inequities among transgender people in Aotearoa New Zealand: Findings from the Counting Ourselves survey
Push and pull factors of transgender migration to Aotearoa/New Zealand
Introduction: Current research has primarily drawn on the push–pull theory to explain factors and circumstances that influence global human migration. Within Aotearoa/New Zealand however, the push–pull factors that influence transgender and nonbinary people’s migration are still poorly understood.
Method: Drawing on this gap, we employed the 2022 Counting Ourselves survey data to examine overseas-born transgender people’s migration intentions to Aotearoa, stratified by demographic differences including country of origin, length of stay, and immigration status. A sample of 576 overseas-born transgender people aged 14 and above were included in the survey (M = 29.58, SD = 12.23).
Results: Participants from the Global South, recent migrants, refugees and asylum seekers, and those with a temporary visa or newly secured residency described greater acceptance of their trans identities and promising socioeconomic opportunities as primary pull factors for migrating to Aotearoa, while citing threats to their safety as push factors for leaving their home countries.
Conclusions: Situating these findings within the current context of Aotearoa/New Zealand—specifically persistent concerns related to migrant welfare, exploitation, and racism—we emphasize the need for more culturally responsive policies and support systems to protect trans migrants who relocate to Aotearoa with hopes of a better, safer future.
View the full article: PDF
Reference: Tan, K., Fernandez, C. C., Byrne, J. L., & Veale, J. F. (2025). Push and pull factors for transgender migration to Aotearoa/New Zealand. Psychology of Sexual Orientation and Gender Diversity. Advance online publication. https://doi.org/10.1037/sgd0000888
Eating disorder risk in transgender youth and its association with unmet need for gender-affirming hormone therapy in Aotearoa New Zealand: a cross-sectional study
Introduction: This study aimed to estimate rates and factors associated with eating disorder risk in transgender youth, and to explore the association between this risk and unmet need for gender-affirming hormone therapy (GAHT).
Method: In a national cross-sectional survey of participants aged 14-24 years, the five-item Sick, Control, One stone, Fat, Food (SCOFF) instrument was used to assess eating disorder risk. GAHT demand was self-reported. Modified Poisson regressions were employed to assess risk.
Results: Overall, 1,401 participants were eligible, of whom 1,010 (72.1%) had valid SCOFF scores. Of these, 398 (38.4%) participants met the threshold for eating disorder risk. In adjusted analyses, those aged 14-18 years had an increased prevalence ratio (PR) of eating disorder risk compared with their counterparts aged 19-24 years (PR: 1.26; 95% confidence interval: 1.06-1.50). GAHT demand was reported by 645 participants, with 277 (42.9%) having unmet need. No statistical evidence was found relating unmet GAHT need with eating disorder risk (p=0.29).
Conclusions: Nearly two in five transgender youth are at eating disorder risk, and unmet GAHT need rates appear higher. While it is recognised that eating disorders are a global health concern, they have not received the priority they deserve. In the calls for urgent action, transgender youth deserve particular attention.
View the full article: PDF
Reference: Davison, M., Veale, J., Byrne, J., Bentham, R., & Schluter, P. (2025). Eating disorder risk in transgender youth and its association with unmet need for gender-affirming hormone therapy in Aotearoa New Zealand: a cross-sectional study. The New Zealand medical journal, 138(1623), 38-52.
The glue that binds us: The positive relationships between whanaungatanga (belonging), the wellbeing, and identity pride for takatāpui who are trans and non-binary
Introduction: This article explores how belonging can enhance well-being for takatāpui (a traditional Māori term that embraces all Māori with diverse genders, sexualities, and sex characteristics) who are trans and non-binary across a range of contexts.
Method: We drew data from the 2018 Counting Ourselves, a nationwide community-based survey of trans and non-binary people in Aotearoa (New Zealand) (N = 1178); of which 161 (13.7%) identified as Māori, the Indigenous people of Aotearoa.
Results: Based on generalised regression models, feelings of belonging with friends, takatāpui communities, Māori communities, and work communities were correlated to higher feelings of life satisfaction, life worthwhileness, and identity pride for takatāpui who are trans and non-binary. In Te Ao Māori (the Māori worldview), such concepts of belonging and relationships are collectively known as whanaungatanga.
Conclusions:Our findings affirm whanaungatanga as foundational to well-being among trans Māori people, enabling them to locate themselves within nurturing and supportive networks. Whanaungatanga is a key policy agenda, alongside other system-level change, that is needed to buffer takatāpui who are trans and non-binary from poverty, stigma, and racism they face. This will require changes to the current policy and practice context. We argue that whanaungatanga, while an important strategy of well-being for trans and non-binary people, must also occur alongside wider system transformations to address transphobia, racism, and cisheteronormativity.
View the full article: PDF or via the publisher
Reference: Hamley, L., Kerekere, E., Nopera, T., Tan, K., Byrne, J., Veale, J., & Clark, T. (2025). The glue that binds us: The positive relationships between whanaungatanga (belonging), the wellbeing, and identity pride for takatāpui who are trans and non‐binary. Health Promotion Journal of Australia, 36(1). https://doi.org/10.1002/hpja.890
Perceived legal protection and institutional trust predict a lower psychological distress level for transgender people in Aotearoa/New Zealand
Background: Few studies have assessed the role of legal protection and institutional trust as structural determinants of health among trans people.
Aim: This study investigated the responses of a nationwide survey of trans people in Aotearoa New Zealand to examine the interplay among perceived legal protection, trust toward institutions, and psychological distress.
Method: Data were employed from the 2018 Counting Ourselves survey (n = 863; Mage = 30.3).We conducted chi-square analyses to identify the extent of differences for institutional trustbetween trans participants and the Aotearoa/New Zealand general populations. Correlation and mediation analyses were utilised to determine whether structural determinants were associated with lower psychological distress levels.
Findings: Our results revealed that over a quarter (26%) of trans participants did not feel New Zealand law protects against discrimination for being trans or non-binary. Trans participants reported heightened levels of distrust compared to the general populations across media (65% vs 39%; RR= 1.66) parliament (52% vs 25%; RR = 2.07), police (49% vs 7%;RR = 7.48), and courts (48% vs 13%; RR = 3.84). Significant demographic differences in institutional trust levels were observed, with younger individuals, trans men, non-binary people assigned female at birth, or people with a disability status reporting lower trust toward different institutions. Perceived legal protection and confidence were correlated with lower psychological distress levels, and institutional trust partially mediated this association.
Conclusions: Findings from this study demonstrate the urgency for government agencies to consult appropriately and work collaboratively with trans communities to identify current gaps in laws and policies that protect the human rights of trans people. Trans-inclusive policies have the potential to elevate community trust toward institutions and improve the meaningful participation of trans people and address inequities.
View the full article: PDF or via the publisher
Reference: Byrne, J. L., Tan, K., Polkinghorne, T. H., Ker, A., Bailey, S., & Veale, J. F. (2024). Perceived legal protection and institutional trust predict a lower psychological distress level for transgender people in Aotearoa/New Zealand. International Journal of Transgender Health, 1-15.
“It’s just a general lack of awareness, that breeds a sense that there isn’t space to talk about our needs”: Barriers and facilitators experienced by transgender people accessing healthcare in Aotearoa/New Zealand
Introduction: Transgender people face serious health disparities associated with underlying social determinants, such as unmet healthcare needs and negative experiences with healthcare providers. Healthcare accessibility dimensions include availability, approachability, acceptability, affordability, and appropriateness. This study aimed to identify the perceived barriers and facilitators that transgender people in Aotearoa/New Zealand experience within these dimensions, as few studies have explored multiple dimensions of healthcare access for transgender people using a large national sample.
Method: Responses to an open-text question in the Counting Ourselves survey (n = 236) were analyzed utilizing qualitative content analysis. A primarily deductive approach was used to identify categories and frame these within a comprehensive healthcare accessibility model.
Results: In line with international research, some prominent barriers were the lack of trans-competent providers (availability/accommodation), experiences of mistreatment (acceptability/appropriateness), and gatekeeping practices (approachability). Facilitators included, among others, providers’ willingness to educate themselves (availability/accommodation), an affirming attitude (acceptability/appropriateness), and competence in navigating services (approachability).
Conclusions: Transgender people in Aotearoa/New Zealand see their healthcare experiences affected by barriers across all dimensions of healthcare access. This highlights a great degree of mismatch between their needs and the healthcare system’s characteristics, thereby breaching their right to healthcare of adequate standards. We recommend that all healthcare practitioners and administrative staff receive training on transgender health, that there is increased accessibility to information on gender-affirming care services, and that collaborative referral procedures that respect patient decisions are implemented.
View the full article: PDF or via the publisher
Reference: González, S., & Veale, J. F. (2024). “It’s just a general lack of awareness, that breeds a sense that there isn’t space to talk about our needs”: Barriers and facilitators experienced by transgender people accessing healthcare in Aotearoa/New Zealand. International Journal of Transgender Health, 26(3), 640–660. https://doi.org/10.1080/26895269.2024.2303476
Transgender-related stigma and gender minority stress-related health disparities in Aotearoa New Zealand: Hypercholesterolemia, hypertension, myocardial infarction, stroke, diabetes, and general health
Background: Research has found that transgender-related enacted stigma—including discrimination, harassment, violence, cyberbullying, community rejection, and conversion efforts—is associated with negative mental health among transgender people. Transgender people also experience physical health disparities that could be due to chronic gender minority stress caused by stigma and prejudice.
Methods: We compared a large New Zealand national survey of transgender participants with the New Zealand Health Survey (NZHS) with age and ethnicity weightings on stress-related health conditions and indicators. We conducted multivariate logistic regression to test associations between transgender-related enacted stigma and physical health conditions and indicators, controlling for age, gender, ethnicity, gender affirming hormone use, and alcohol and tobacco use.
Findings: Transgender participants had a greater likelihood of ever having hypertension (63%, 95% CI 41%–89%), a myocardial infarction (98%, 6%–271%), a stroke (104%, 2%–311%), hypercholesteremia 148% (114%–188%), and current poor or fair general health (128%, 107%–151%). There were no significant differences for diabetes. Compared with those scoring at the 10th percentile on transgender-related enacted stigma, those at the 90th percentile were more likely to have had hypertension (81%, 36%–140%), hypercholesteremia (54%, 20%–98), and poor/fair health (75%, 45%–110%).
Interpretation: We found large disparities for stress-related physical health conditions and indicators, and transgender people who experienced higher transgender-related enacted stigma had a significantly increased prevalence of these negative outcomes. Our findings highlight the need for health professionals to consider gender minority stress and for interventions and policy/law reforms to address transgender-related stigma.
View the full article: PDF or via the publisher
Reference: Veale, J.F (2023) Transgender-related stigma and gender minority stress-related health disparities in Aotearoa New Zealand: hypercholesterolemia, hypertension, myocardial infarction, stroke, diabetes, and general health. The Lancet Regional Health-Western Pacific, e100816. DOI: 10.1016/j.lanwpc.2023.100816
Uptake, experiences and barriers to cervical screening for trans and non-binary people in Aotearoa New Zealand
Background: Little is known about experiences and barriers for trans and non- binary (TGNB) people eligible for cervical screening in Aotearoa New Zealand.
Aims: To identify uptake, barriers and reasons for delaying cervical cancer screening among TGNB people in Aotearoa.
Materials and Methods: The 2018 Counting Ourselves data on TGNB people assigned female at birth aged 20– 69 years who had ever had sex, were analysed to report on experiences of those who were eligible for cervical screening (n = 318). Participants answered questions about whether they had taken part in cervical screening and reasons behind any delays in receiving the test.
Results: Trans men were more likely than non- binary participants to report that they did not require cervical screening or were unsure if they needed it. For those who had delayed cervical screening, 30% did so due to feeling worried about how they would be treated as a trans or non- binary person and 35% due to another reason. Other reasons for delay related to general and gender- related discomfort, previous traumatic experiences, anxiety or fear of the test and pain. Material bar-riers to access included cost and lack of information.
Conclusions: The current cervical screening program in Aotearoa does not con-sider the needs of TGNB people, leading to delayed and reduced uptake of cervical screening. Health providers require education on the reasons TGNB people delay or avoid cervical screening in order to provide appropriate information and affirmative healthcare environments. The human papillomavirus self- swab may address some of the existing barriers.
View the full article: PDF or via the publisher
Reference: Carroll, R., Tan, K.K.H., Ker, A., Byrne, J.L., & Veale, J.F (2023) Uptake, experiences and barriers to cervical screening for trans and non-binary people in Aotearoa New Zealand. Australian and New Zealand Journal of Obstetrics and Gynaecology, 63(3), 448-453. DOI: 10.1111/ajo.13674
Unmet need for gender-affirming care as a social determinant of mental health inequities for transgender youth in Aotearoa/New Zealand
Background: Past studies have demonstrated better mental health and well-being among transgender youth who had accessed gender-affirming care. However, few existing studies have assessed unmet need for gender-affirming care as a social determinant of mental health inequities.
Methods: Data on unmet need for gender-affirming care, distress and suicidality were analysed from the 2018 Counting Ourselves nationwide community-based survey of transgender people in Aotearoa/New Zealand. Associations between unmet need for gender-affirming care and mental health indicators were tested for transgender youth within the sample (aged 14–26 years; n = 608; Mage = 20.5).
Results: Transgender youth reported unmet needs ranging from 42% for gender-affirming hormone to 100% for feminizing surgeries and
voice surgeries. Overall unmet need for gender-affirming care was associated with worse mental health. Trans men with an unmet need for chest reconstruction (84%) scored an average of 7.13 points higher on the K10 Psychological Distress Scale relative to those whose need had been met. Participants reporting unmet need for hormones (42%) had twice the odds (adjusted odds ratios = 2.01; CI = 1.02–3.98) of having attempted suicide in the last 12 months.
Conclusions: Dismantling barriers to accessing gender-affirming care could play a crucial role in reducing mental health inequities faced by transgender youth.
View the full article: PDF or via the publisher
Reference: Tan, K.K.H., Byrne, J.L., Treharne, G.J. & Veale, J.F (2023). Unmet need for gender-affirming care as a social determinant of mental health inequities for transgender youth in Aotearoa/New Zealand. Journal of Public Health (Oxf), 45(2):e225-e233. DOI: 10.1093/pubmed/fdac131.
PrEP awareness and protective barrier negotiation among transgender people attracted to men in Aotearoa New Zealand
Introduction: Internationally, trans women are disproportionately impacted by HIV, encounter specific barriers navigating safer sex and face inequities accessing HIV prevention, including pre-exposure prophylaxis (PrEP). Aotearoa/New Zealand (hereafter Aotearoa) was one of the first countries internationally to publicly fund PrEP in 2018, including for trans people. However, few data exist on PrEP awareness or sexual negotiation among trans populations to guide implementation. We present the first Aotearoa data on trans people’s ability to negotiate barrier protection and awareness of PrEP efficacy and availability.
Methods: We used data from a large, diverse community-based nationwide survey of trans (including non-binary) people in Aotearoa: Counting Ourselves (N = 1178) conducted from 21 June to 30 September 2018. Generalized regression analyses were carried out among participants who have had sex (n = 704; Mage = 32.5) to identify associations between demographic factors (age, gender and sexual attraction, ethnicity, income, education qualification and current sex work involvement) and the Trans-Specific Barrier Negotiation Self-Efficacy (T-Barrier) Scale and PrEP awareness.
Results: The mean value of a 40-point T-Barrier Scale was 33.45 (SD: 6.89), suggesting a relatively high perceived ability among our participants to negotiate protective barrier usages in different situations. Asian participants scored 3.46 points lower compared to Pākehā (White) participants, and trans women attracted to men (cisgender and/or trans men) scored 2.40 points higher than trans women not attracted to men. Three-fifths (59.7%) were aware that PrEP reduced HIV risks and did not prevent sexually transmitted infections (STI) transmission, and only two-fifths (40.2%) knew PrEP was publicly funded for trans people. In multivariate models, we found participants who were older, trans women or those with lower education qualifications were less likely to have increased levels of PrEP awareness.
Conclusion: Participants attracted to men have a higher potential need for PrEP and were more likely to report PrEP awareness and that they could negotiate protective barrier usage. However, trans women and those with lower educational qualifications reported lower levels of PrEP awareness. More trans-competent sexual health education, drawing on the newly released PrEP guidelines, is needed to promote the benefits of PrEP in the Aotearoa HIV epidemic context, particularly for trans women.
View the full article: PDF or via the publisher
Reference: Byrne, J.L., Tan, K.K.H., Saxton, P.J., Bentham, R.M. & Veale, J.F (2022). PrEP awareness and protective barrier among transgender people attracted to men in Aotearoa New Zealand. Journal of the International AIDS Society, 25(S5), e25980. DOI: 10.1002/jia2.25980
Barriers to possessing gender-concordant identity documents are associated with transgender and nonbinary people’s mental health in Aotearoa/New Zealand
Purpose: This study sought to expand on previous scholarship focused on gender-concordant identity documents (IDs) as a social determinant of health. We examined the association between barriers to legal gender recognition and the mental health of transgender and nonbinary people in Aotearoa/New Zealand.
Methods: We used data from a 2018 nationwide community-based survey of trans and nonbinary people in Aotearoa (N= 818). Variables of investigation included: gender-concordant IDs, mental health (past-month psychological distress, past-year nonsuicidal self-injury, past-year suicidality) and barriers to changing gender markers on a birth certificate or passport. Associations between gender-concordant IDs and mental health were determined using generalized linear regression models.
Results: In total, 34.8% reported the correct name on all of their IDs. The proportion with the correct gender marker on both birth certificates and passports was 16.0%. Participants with gender-concordant IDs were more likely to be older, have higher levels of income and education, and have had genital reconstruction. In addition, 68.7% of participants reported experiencing at least one barrier to changing gender markers on their IDs, and these participants had significantly higher average points of psychological distress scores (b = 2.39) and greater odds of suicidal ideation (odds ratio = 2.02) than those with gender-concordant IDs, after adjusting for sociodemographic variables.
Conclusion: We present novel findings on higher levels of mental health problems among trans and nonbinary people who faced barriers in trying to obtain gender-concordant IDs compared with those with gender-concordant IDs. Removing barriers to legal gender recognition may be an effective way to improve mental health.
View the full article: PDF or via the publisher
Reference: Tan, K.K.H., Watson, R.J., Byrne, J.L. & Veale, J.F (2022) Barriers to possessing gender-concordant identity documents are associated with transgender and nonbinary people’s mental health in Aotearoa/New Zealand. LGBT Health, 9(6), 401-410. DOI: 10.1089/lgbt.2021.0240
“I teach them. I have no choice”: Experiences of primary care among transgender people in Aotearoa New Zealand.
Aim: This study aims to report primary care experiences among transgender people in Aotearoa New Zealand based on quantitative and qualitative data from a nationwide community-based survey of transgender people.
Methods: Subsamples with a usual general practitioner were employed from the 2018 Counting Ourselves Survey (n=871) and the 2018/19 New Zealand Health Survey to assess inequities between these samples in primary care experiences and barriers. Guided by Andersen’s Behavioural Model of healthcare access, we conducted a content analysis on comments from Counting Ourselves participants (n=153) to identify themes about issues of concern for transgender people when accessing primary care.
Results: Transgender participants had greater risk of feeling no confidence in their GPs (Mdifference=0.22; Cohen’s d=0.39), reporting barriers accessing primary care due to cost (38.4% vs 17.4%; RR=2.21), and transport issues (13.5% vs 3.0%; RR=4.58) compared to the general population. Content analysis uncovered how transgender people’s primary care experiences are shaped by healthcare environments, predisposing characteristics, and enabling resources.
Conclusion: Our findings indicate ways to ensure primary care services are inclusive so that all transgender people feel welcome. This requires all primary healthcare professionals to demonstrate core trans-specific cultural safety when providing healthcare to transgender patients.
View the full article: PDF or via the publisher
Reference: Tan, K.K.H., Carroll, R., Treharne, G.J., Byrne, J.L. & Veale, J.F (2022) “I teach them. I have no choice”: Experiences of primary care among transgender people in Aotearoa New Zealand. New Zealand Medical Journal, 135(1559), 59-72.
Supportive interactions with primary care doctors are associated with better mental health among transgender people: results of a nationwide survey in Aotearoa/New Zealand
Background: Past research has established that transgender people experience significant disparities in mental health outcomes and healthcare dissatisfaction compared with cisgender people, but more research is needed on how supportive healthcare interactions relate to the mental health of transgender people.
Objectives: The 2 main aims of our analyses were: (i) to establish the most common negative experiences in healthcare and the most common supportive experiences specifically with primary care doctors for transgender people; and (ii) to examine the association of supportive experiences with mental health variables after controlling for demographic factors.
Methods: Data from the 2018 Counting Ourselves nationwide survey of transgender people were analysed using regression modelling. The 948 participants with a primary care doctor or general practitioner were included in analyses. Participants were aged 14–83 years old (mean 30.20).
Results: The most common supportive experiences involved primary care doctors treating transgender people equitably, with competence, and with respect. Participants with more negative healthcare experiences had higher psychological distress as well as higher likelihood of reporting nonsuicidal self-injury and suicidality. Conversely, participants with more experiences of supportive primary care doctors had lower psychological distress and were less likely to have attempted suicide in the past 12 months.
Conclusion: When transgender people receive supportive care from their primary care providers they experience better mental health, despite ongoing negative healthcare experiences. Future research is needed to confirm ways of supporting positive trajectories of mental health for transgender people but these findings demonstrate the importance of positive aspects of care.
View the full article: PDF or via publisher
Reference: Treharne, G.J., Carroll, R., Tan, K.K.H. & Veale, J.F (2022) Supportive interactions with primary care doctors are associated with better mental health among transgender people: results of a nationwide survey in Aotearoa/New Zealand. Family Practice, 39(5), 834-842. DOI: 10.1093/fampra/cmac005
Gender identity change efforts faced by trans and non-binary people in New Zealand: Associations with demographics, family rejection, internalized transphobia, and mental health
Based on their transphobic assumption that being transgender or non-binary (TNB) is pathological or otherwise undesirable, gender identity change efforts (GICE) attempt to make a person’s gender conform with their sex assigned at birth. While many professional bodies have noted that GICE practices are unethical, there has been little empirical research into the prevalence and correlates of GICE exposure. Counting Ourselves: the Aotearoa New Zealand Trans and Non-binary Health Survey is a community-based study, which participants completed mostly online. Out of 610 participants who had ever spoken to a health professional about their gender, 19.7% [16.6%, 23.1%] reported GICE exposure and a further 9.3% [7.2%, 11.9%] did not know. GICE exposure was higher among younger participants. Participants with GICE exposure were more likely than those without such exposure to report psychological distress, non-suicidal self-injury (NSSI), suicidal ideation, and suicide attempts (e.g., suicidal ideation OR = 2.39). GICE partially mediated the effect of family rejection on mental health and Internalized Transphobia partially mediated the effect of GICE on mental health. These correlates between GICE and mental health replicate recent findings from the US Trans Survey, and the mediation analyses help to understand potential causal mechanisms underlying these correlations. Although our findings are limited by being a convenience sample, they are consistent with the hypothesis that GICE exposure is harmful to TNB people’s mental health. Moreover, these findings support moves by many professional bodies to emphasize that GICE is unethical and the legal steps taken by a growing number of jurisdictions to ban such practices.
View the full article: PDF or via the publisher
Reference: Veale, J.F., Tan, K.K.H. & Byrne, J.L (2022) Gender identity change efforts faced by trans and non-binary people in New Zealand: Associations with demographics, family rejection, internalized transphobia, and mental health. Psychology of Sexual Orientation and Gender Diversity, 9(4), 478-487. DOI: 10.1037/sgd0000537
Access to fertility preservation for trans and non-binary people in Aotearoa New Zealand
There is a growing need for healthcare professionals to discuss fertility preservation options with trans and non-binary people before commencing medical transition as part of informed consent-based models of care. In this article, we adapt the Five-A framework of healthcare access to examine fertility preservation information and services. To do so, we present an analysis of data from Counting Ourselves, the first comprehensive national survey in Aotearoa New Zealand of trans and non-binary people’s health and the first study exploring their access to cryopreservation information and services. Among 419 participants who had received gender-affirming hormones or surgery, 33.7% received information about options for fertility preservation and 15.8% accessed fertility preservation services. Findings from the study indicate the need for greater understanding of trans and non-binary people’s desire for genetically related children, and what type of information and form of delivery would be most helpful to ensure equitable outcomes in relation to decision-making around fertility and future family-building.
View the full article: PDF or via the publisher
Reference: Ker, A., Shaw, R.M., Byrne, J.L., & Veale, J.F. (2022) Access to fertility preservation for trans and non-binary people in Aotearoa New Zealand. Culture, Health & Sexuality, 24(9), 1273-1288. DOI: 10.1080/13691058.2021.1944670
“Being trans intersects with my cultural identity”: Social determinants of mental health among Asian transgender people
Purpose: While studies on the relationship between social determinants and mental health among transgender people in Asia are increasing, there is a paucity of research on Asian transgender people living in Western countries. This study aimed to examine how social positions (gender, ethnicity, and migrant status) and social determinants of mental health were inter-related for Asian transgender people in Aotearoa/New Zealand.
Methods: We analysed both quantitative and qualitative data from Asian participants (n = 49) who responded to the 2018 Counting Ourselves: Aotearoa New Zealand Trans and Non-Binary Health Survey.
Results: Overall, 35% reported a very high psychological distress level. There were high levels of unmet needs for gender-affirming care, and participants reported a range of negative experiences at health care settings. About two-fifths had been discriminated because of their transgender (42%) or Asian (39%) identities. Fewer than half of participants felt that their family members were supportive of them being transgender (44%), and most reported they had supportive friends (73%). More than two-thirds of participants (68%) had a strong sense of belongingness to the transgender community and 35% reported this for the Asian community. Qualitative findings revealed specific challenges that participants experienced; these included barriers to accessing health care due to their migrant status and language barriers, influences of Asian cultures on mental health experiences, and rejection by family and people in Asian communities.
Conclusion: Our study provides evidence for health care providers, researchers, and policy makers to employ a culturally appropriate lens to improve knowledge about the intersectional experiences of being Asian and transgender.
View the full article: PDF or via the publisher
Reference: Tan, K.K.H., Yee, A., & Veale, J.F. (2022) “Being trans intersects with my cultural identity”: Social determinants of mental health among Asian transgender people. Transgender Health, 7(4), 329-339. DOI:10.1089/trgh.2021.0007
“It’s how the world around you treats you for being trans”: Mental health and wellbeing of transgender people in Aotearoa New Zealand
Globally, transgender people have been described as a highly marginalised population due to cisgenderism that delegitimises their gender identities and expressions. Despite robust evidence from many countries noting the association of discrimination and stigma for being transgender with heightened mental health risks, qualitative research that examines the nuances of mental health indicators using health equity frameworks has been scant both in Aotearoa/New Zealand and overseas. Using an inductive thematic approach, this paper analysed 222 open-text responses in the mental health section of the 2018 Counting Ourselves: Aotearoa New Zealand, Trans and Non-binary Health Survey. Our findings showed four overarching themes: gender-affirming healthcare, mental healthcare services and accessibility, gender minority stress, and self-affirmation and social support. Participants’ narratives described pervasive gender minority stress experiences in gender-affirming and mental healthcare services, including unmet healthcare needs, lack of competency in healthcare delivery, and pathologisation of their genders. In social settings, our participants commonly reported discrimination and violence, although they also reported that self-affirmation strategies and social support offset the impacts of gender minority stress on their mental health. The current findings indicate the importance of exploring mental health outcomes for transgender people in relation to cisgenderism and resultant gender minority stress.
View the full article: PDF or via the publisher
Reference: Tan, K.K.H., Schmidt, J.M., Ellis, S.E., Veale, J.F., & Byrne, J.L. (2022) ‘It’s how the world around you treats you for being trans’: mental health and wellbeing of transgender people in Aotearoa New Zealand, Psychology & Sexuality. 13(5), 1109-1121. DOI: 10.1080/19419899.2021.1897033
Enacted stigma experiences and protective factors are strongly associated with mental health outcomes of transgender people in Aotearoa/New Zealand
Introduction: International evidence has found large mental health inequities among transgender people and demonstrates that mental health outcomes are associated with enacted stigma experiences and protective factors. This study aimed to examine the extent of associations of enacted stigma experiences specific to transgender people alongside protective factors with mental health of transgender people in Aotearoa/New Zealand.
Method: The 2018 Counting Ourselves survey was a nationwide community-based study of transgender people (N = 1,178, Mage = 29.5) living in Aotearoa/New Zealand. The survey assessed a wide range of gender minority stress experiences and protective factors that comprised primary (support from friends and family) and secondary social ties (neighbourhood and transgender community belongingness). We calculated the predicted probabilities that transgender people exhibit very high psychological distress level, non-suicidal self-injury, and suicidal risks with different combinations and exposure profiles of enacted stigma and protective factors.
Results: Our findings demonstrated that enacted stigma was associated with negative mental health, and support of friends and family was linked to better outcomes across all mental health measures. Beyond primary social ties, sense of belongingness to neighbourhood and transgender communities were linked to reduced odds of psychological distress and suicidal ideation. For those scoring high on enacted stigma and low on protective factors, our model revealed a 25% probability of attempting suicide in the last year compared to 3% for those scoring low on enacted stigma and high on protective.
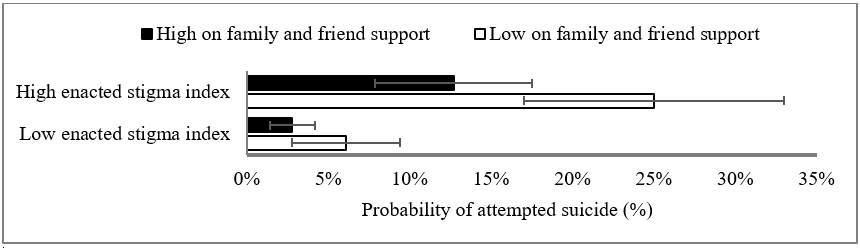
Conclusions: Echoing previous findings, this study demonstrates that transgender people across Aotearoa/New Zealand are less likely to manifest life-threatening mental health outcomes if they experience low levels of enacted stigma and high levels of access to protective factors. Our findings suggest a need to address the enacted stigma that transgender people face across interpersonal and structural settings, and also to enhance social supports that are gender affirmative for this population.
View the full article: PDF or via the publisher
Reference: Tan, K. K. H., Treharne, G. J., Ellis, S. J., Schmidt, J. M., & Veale, J. F. (2021). Enacted stigma experiences and protective factors are strongly associated with mental health outcomes of transgender people in Aotearoa/New Zealand. International Journal of Transgender Health, 22(3), 269-280. DOI: 10.1080/15532739.2020.1819504
Mental Health inequities among transgender people in Aotearoa New Zealand: Findings from the Counting Ourselves Survey
There has been little international research looking at differences in mental health across different age groups. This study examines mental health inequities between transgender people and the Aotearoa/New Zealand general population from youth to older adulthood. The 2018 Counting Ourselves survey (N = 1178) assessed participants’ mental health using the Kessler Psychological Distress Scale (K10) and diagnoses of depression and anxiety disorders, questions that were the same as those used in the New Zealand Health Survey. Our results showed significant mean score differences for transgender people on K10, and these differences were almost two standard deviations higher than the general population (Cohen’s d = 1.87). The effect size differences, however, decreased from youth to older adults. Regression analyses indicated trans women were less likely to report psychological distress than trans men and non-binary participants. There was an interaction effect for age and gender, with lower psychological distress scores found for younger trans women but higher scores for older trans women. The stark mental health inequities faced by transgender people, especially youth, demonstrate an urgent need to improve the mental health and wellbeing of this population by implementing inclusive institutional practices to protect them from gender minority stress.
View the full article: PDF or via the publisher
Reference: Tan, K. K. H., Ellis, S. J., Schmidt, J. M., Byrne, J. L., & Veale, J. F. (2020). Mental health inequities among transgender people in Aotearoa New Zealand: Findings from the Counting Ourselves survey. International Journal of Environmental Research and Public Health, 17(8), 262. DOI: 10.3390/ijerph17082862
